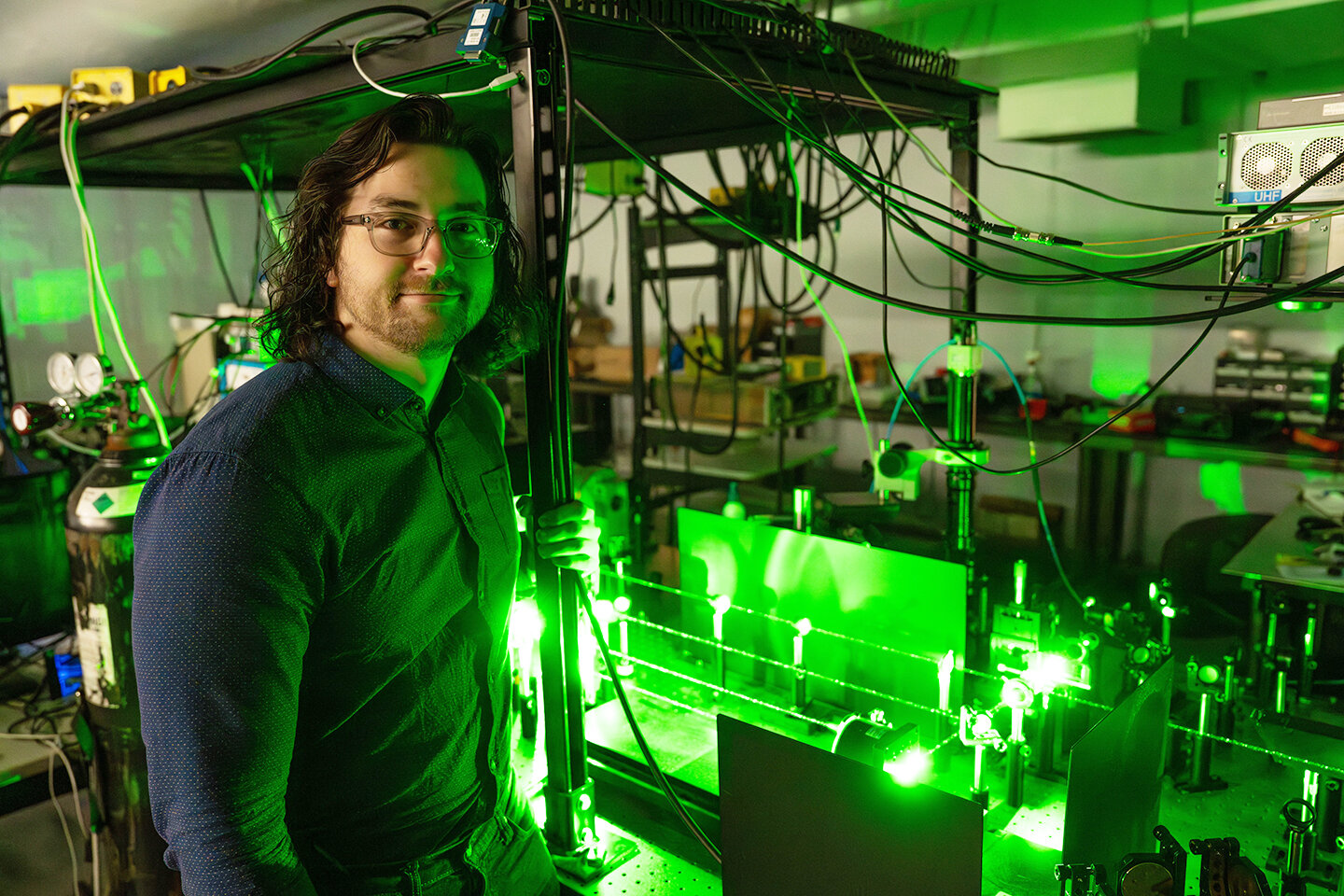
Valentin Fuster, MD, PhD. “REBOOT Trial” shows beta blockers—drugs commonly prescribed for heart attacks—may offer no clinical benefit for these patients. Credit: Mount Sinai Health System
A drug with a decades-long influence
Beta-blockers have been a staple of cardiovascular care for decades. By dampening the heart’s response to adrenaline, these drugs slow the heartbeat, lower blood pressure, and reduce the heart’s oxygen demand. For many patients, that creates relief from chest pain, steadier heart rhythms, and better exercise tolerance. But as medicine advances and patients live longer with chronic conditions, clinicians are reexamining how these drugs fit into long-term, stable heart disease.
What the latest voices are saying
Recent reviews and guideline discussions are prompting clinicians to rethink “one-size-fits-all” long-term beta-blocker use. In stable heart disease—where symptoms are controlled and major events are infrequent—the long-term benefit of continuing beta-blockers for every patient is being questioned. Some researchers argue that the best approach is more individualized: continue therapy when benefits are clear and monitor closely when symptoms have settled, side effects arise, or additional therapies could offer similar protection with different risks.
It’s important to recognize what beta-blockers do well and where they may have diminishing returns. For patients with heart failure with reduced ejection fraction (a specific, serious form of heart disease), beta-blockers remain a cornerstone due to solid evidence of mortality and symptom improvement. But for stable conditions such as uncomplicated hypertension or stable coronary artery disease without other complications, the advantage over time may hinge on the patient’s unique profile, tolerability, and other treatments in their toolbox.
Who benefits, and who should be watched closely
Beneficiaries
People with certain conditions—like heart failure with reduced ejection fraction, specific rhythm disorders, or post-event scenarios where the drug’s stabilizing effects reduce risk—often continue to gain meaningful benefit from beta-blockers.
Cautionary cases
Some individuals experience fatigue, dizziness, sexual side effects, or bronchospasm (particularly if they have reactive airways). In such cases, the ongoing risk-benefit balance may tilt toward tapering, adjusting the dose, or trying alternative therapies.
Withdrawal awareness
Stopping a beta-blocker abruptly can occasionally trigger a rebound increase in heart rate or chest pain. If a clinician decides to reduce or discontinue use, it’s usually done gradually under medical supervision.
Guidelines and the shift toward personalization
Major cardiology guidelines increasingly emphasize patient-centered decisions. They encourage clinicians to:
Regular reassessment
Reassess the ongoing need for beta-blockers at regular intervals, especially in patients with long-standing stable disease.
Consider coexisting conditions
Consider conditions such as COPD or asthma, where beta-blockers can pose respiratory risks, when choosing therapies.
Weigh alternatives and complements
Weigh alternatives and complements, including other anti-anginal or antihypertensive options, lifestyle changes, and risk-factor management.
This nuanced approach aims to preserve heart health while minimizing side effects and unnecessary medication burden. It reflects a broader trend in medicine: tailoring treatment to the individual rather than applying blanket recommendations to all patients with a given diagnosis.
What this means for patients today
If you’ve been taking a beta-blocker for years and feel well, it doesn’t automatically mean you should stop. The decision to continue, adjust, or discontinue should be made in close collaboration with your healthcare provider, considering:
- Your current symptoms and activity level
- Blood pressure, heart rate, and other markers
- Side effects impacting daily life
- The presence of other conditions that may influence drug choice
For people starting therapy, the focus remains on selecting the right drug for the right indication, with a plan for regular reassessment as health status evolves. Alongside medications, non-drug strategies—such as heart-healthy eating, physical activity appropriate to your condition, and smoking cessation—continue to play a pivotal role in reducing cardiovascular risk.
A look at the broader science landscape
This conversation about beta-blockers sits within a larger reexamination of long-term pharmacotherapy in chronic diseases. As new drugs enter the market and precision medicine advances, clinicians increasingly balance historical benefits against potential long-term harms. The goal is not to abandon proven therapies, but to use them thoughtfully—maximizing benefit while minimizing downsides.
Conclusion and curiosity cue
The story of beta-blockers over the past 40 years is one of both success and humility: a reminder that medicine improves in layers—built on proven benefits, refined by new evidence, and personalized to each patient’s journey. As science continues to evolve, what other familiar medicines might reveal new faces or refined roles? Share your thoughts or experiences with beta-blockers in the comments below.
Call to action / curiosity-sparking question
If a well-tolerated beta-blocker has supported your health for years, would you consider a formal review of your regimen to confirm it still fits your goals and risks? Why or why not?
“Beta-Blockers after Myocardial Infarction without Reduced Ejection Fraction” by Borja Ibanez, Roberto Latini, Xavier Rossello, Alberto Dominguez-Rodriguez, Felipe Fernández-Vazquez, Valentina Pelizzoni, Pedro L. Sánchez, Manuel Anguita, José A. Barrabés, Sergio Raposeiras-Roubín, Stuart Pocock, Noemí Escalera, Lidia Staszewsky, Carlos Nicolás Pérez-García, Pablo Díez-Villanueva, Jose-Angel Pérez-Rivera, Oscar Prada-Delgado, Ruth Owen, Gonzalo Pizarro, Onofre Caldes, Sandra Gómez-Talavera, José Tuñón, Matteo Bianco, Jesus Zarauza, Alfredo Vetrano, Ana Campos, Susana Martínez-Huertas, Héctor Bueno, Miguel Puentes, Giulietta Grigis, Juan L. Bonilla-Palomas, Elvira Marco, José R. González-Juanatey, Roi Bangueses, Carlos González-Juanatey, Ana García-Álvarez, Juan Ruiz-García, Anna Carrasquer, Juan C. García-Rubira, Domingo Pascual-Figal, Carlos Tomás-Querol, J. Alberto San Román, Pasquale Baratta, Jaume Agüero, Roberto Martín-Reyes, Furio Colivicchi, Rosario Ortas-Nadal, Pablo Bazal, Alberto Cordero, Antonio Fernández-Ortiz, Pierangelo Basso, Eva González, Fabrizio Poletti, Giulia Bugani, Marzia Debiasio, Deborah Cosmi, Alessandro Navazio, Javier Bermejo, Giovanni Tortorella, Marco Marini, Javier Botas, José M. de la Torre-Hernández, Filippo Ottani and Valentín Fuster, 29 August 2025, New England Journal of Medicine.
DOI: 10.1056/NEJMoa2504735
“Beta-blockers after myocardial infarction: effects according to sex in the REBOOT trial” by Xavier Rossello, Alberto Dominguez-Rodriguez, Roberto Latini, Pedro L Sánchez, Sergio Raposeiras-Roubín, Manuel Anguita, José A Barrabés, Giulietta Grigis, Ruth Owen, Stuart Pocock, Sandra Gómez-Talavera, Ines García-Lunar, Noemí Escalera, Carlos Nicolás Pérez-García, Stefania Angela Di Fusco, Gonzalo Pizarro, María López Benito, Giulia Pongetti, Luis M Rincón-Díaz, Irene Buera, José Rozado, María Jesús García, Oscar Prada-Delgado, Deborah Cosmi, Valentín Fuster and Borja Ibanez, 30 August 2025, European Heart Journal.
DOI: 10.1093/eurheartj/ehaf673